Development of a Wearable Device for PHR Application
Copyright ⓒ 2021 The Digital Contents Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-CommercialLicense(http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.

Abstract
In modern society, the number of elderly people and people with chronic illness who engage in external activities has increased due to advances in medical technology. In the case of elderly people and patients with chronic diseases, temperature changes caused by sudden activities such as external activities due to functional deterioration of the autonomic nervous system are exposed to diseases such as hypothermia, heat stroke, solar radiation disease, and myocardial infarction. In severe cases, it also leads to death. Therefore, in this study, we developed a wearable device so that elderly people and people with chronic illness can monitor sudden physical changes during external activities. Wearable devices have made it possible to measure changes in heart rate, oxygen saturation, and body temperature in real time. The wearable device is XBEE, which communicates with the main controller. The data transfer rate between the wearable device and the main controller was very fast at 24.0ms. As a result of measuring changes in heart rate, oxygen saturation, and body temperature by a healthy person wearing a wearable device, it was confirmed that data transfer was smoothly transmitted.
초록
현대 사회는 의료기술 발전으로 인해 외부 활동을 하는 고령층 및 만성질환자가 증가하였다. 노인 및 만성질환자의 경우 자율신경계 기능 저하로 외부 활동 등의 급격한 활동으로 인한 온도 변화는 저체온증, 열사병, 일사병, 심근경색 등과 같은 질병에 노출이 되고 있으며, 심한 경우 사망으로도 이어지고 있다. 따라서 본 연구에서는 노인 및 만성질환자가 외부활동 시 갑자기 발생하는 신체 변화를 모니터링 할 수 있도록 웨어러블 기기를 개발하였다. 웨어러블 기기는 심박, 산소포화도, 체온 변화를 실시간 측정이 가능하도록 하였다. 웨어러블 기기는 XBEE로 메인컨트롤러와 통신을 하고 데이터가 전송되도록 하였다. 웨어러블 기기와 메인컨트롤러 사이의 데이터 전송속도가 24.0ms로 매우 빨랐다. 정상인이 웨어러블 기기를 착용하고 심박, 산소포화도, 체온변화를 측정한 결과 데이터의 전송이 원활히 전송됨을 확인하였다.
Keywords:
Wearable, Body temperature maintenance device, Heart rate, Oxygen saturation, Body temperature change키워드:
웨어러블, 체온유지장치, 심박, 산소포화도, 체온변화Ⅰ. Introduction
Advancement of modern medicine and improvement in standards of living have increased the average lifespan, and the number of elderly and chronic patients has risen sharply. The elderly and chronic patients are prone to diseases such as hypothermia, heatstroke, cardiac infarction, and digestive disorders owing to hypofunction in the sensing ability that detects a change in body temperature through malfunction of the autonomic nervous system.
Human body can be divided into the core and outer parts. Core temperature remains constant owing to the heat generated through basal metabolism of somatic cells. The outer part serves as an insulator between the core part and the external environment. The heat, generated in the core part through basal metabolism of somatic cells, is carried to the outer part through tissues and blood. The temperature of peripheral areas is kept constant through gain or loss of heat from external environments in the outer part. [1-3] In a healthy body, the core temperature is maintained at approximately 37–38 °C, with a temperature change of 0.5–1 ℃. When the body temperature increases or decreases beyond the said range owing to an abrupt temperature change, the body maintains the temperature through physiological adaptation and behavioral responses. [4]
When hypothermia occurs owing to a decrease in body temperature, the blood vessels in the peripheral tissues constrict, which decreases the blood flow into the peripheral areas and the oxygen supply to the tissues. It mostly occurs in the limbs, rather than in the trunci. [5] The decrease in blood flow degrades local sensing abilities and causes muscle weakness, making the skin cold and pale. When such a condition is maintained for hours without treatment, the body temperature drops below 34.4 °C, and the pulse, respiratory activity, and blood pressure drop to a life-threatening level. [6]
Sunstroke, which can occur during heavy exercises or activities in a high temperature environment, causes dizziness, headache, and nausea. In addition, bodily tissues can be destroyed owing to a high body temperature, and there is a risk of death when the physiological defense function is lost.
In this study, we developed a wearable device that can monitor the heartbeat, blood oxygen, and body temperature by being connected to a body heat keeper [7-9] using a thermoelement, which is employed in various industry sectors for monitoring of the wearer’s health data.
Ⅱ. Biometric Information Measurement
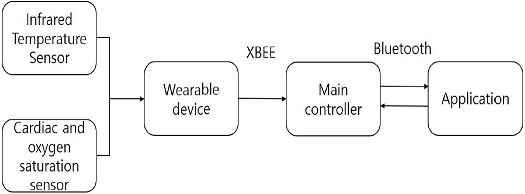
The main controller of the wearable device and body heat keeper transmits and receives data through XBee. The body heat keeper was designed to be turned on and off depending on the body temperature measured by the wearable device. In addition, we developed an application that presents the collected data. The collected data on heartbeat, blood oxygen, and body temperature were transmitted in real time from the main controller to the application using Bluetooth.
The main controller’s MCU was selected considering LCD communication, Zigbee, and Bluetooth communication. USART communication was used for data transmission and reception with LCD, Zigbee, and Bluetooth. For data transmission and reception with a temperature sensor, the 12C port was used.
Figure 1 presents the flow diagram of the biometric data. For measurement of data on a patient’s heartbeat and blood oxygen, a sensor (MAX30102, Maxim integrated, USA) was used. For the measurement of data on the patient’s body temperature, an infrared temperature sensor (MLX90614B, Melexis, Belgium) was used.
Ⅲ. Wearable Device Design and Development
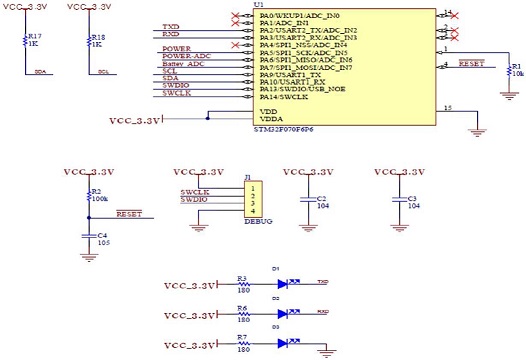
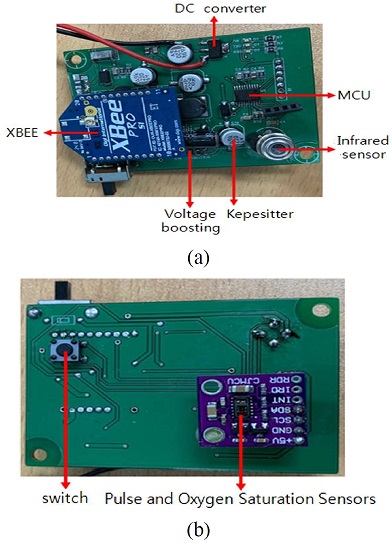
Figure 2 depicts the wearable device’s MCU. It was a STM32F070 MCU, which is equipped with a 32-bit cortex M-0 processor, with a flash memory of 32-128 kB and SRM of 6-16 kB. Figure 3 presents the developed wearable device’s PCB. We connected the infrared temperature sensor and heartbeat and blood oxygen sensor in parallel for simultaneous sensing and used 12C communication to transmit and receive data.
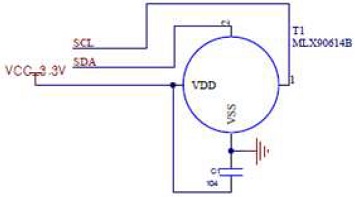
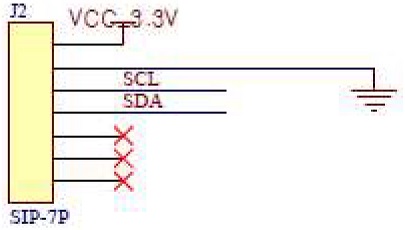
Figure 4 illustrates the circuit diagram of the infrared temperature sensor that was used for real-time contactless body temperature measurement. It is a small sensor that can measure an object’s surface temperature from –70 to +380 °C, with an error of ±0.5 °C and measurement resolution of 0.02 °C. We placed a pull-up resistor on the SCL and SDA pins to improve the accuracy and reliability of 12C communication. The real-time data on body temperature were configured to be transmitted to the main controller using 12C communication.
Figure 5 presents the circuit diagram of the heartbeat and blood oxygen sensor. The characteristics of the sensor are provided in Table 1. The sensor shoots red light and infrared light from the LED and senses the reflection of the lights from the skin to measure the heartbeat and blood oxygen under the skin.
Ⅳ. Experimentation and discussion
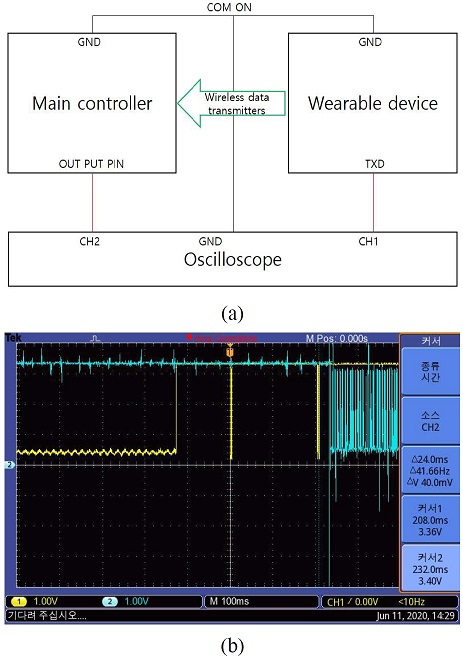
The speed of data transfer between the wearable device and the controller was measured. The block diagram for the measurement of data transfer speed is provided in Figure 6, along with the measured value. We connected oscilloscope CH1 to the data transmitting end (TXD) of the sensor board and oscilloscope CH2 to the main controller. Then, we put the “GND” of the sensor board and oscilloscope to “COM ON.” The sensor board transmits data to the main controller. The main controller sets the output pin to high every time it receives data. The data transfer speed from the wearable device to the controller was measured to be 24.0
To calculate the impact of body heat maintenance on the biometric data, we put on the wearable device and measured the biometric data before and after wearing the body heat keeper.
First, we measured the data at 5 min intervals when we stopped, walked, ran, walked, and stopped in the written order while wearing the wearable device only. Subsequently, we put on the body heat keeper, along with the wearable device, and measured the data at 5 min intervals when we stopped, walked, ran, walked, and stopped in the written order.
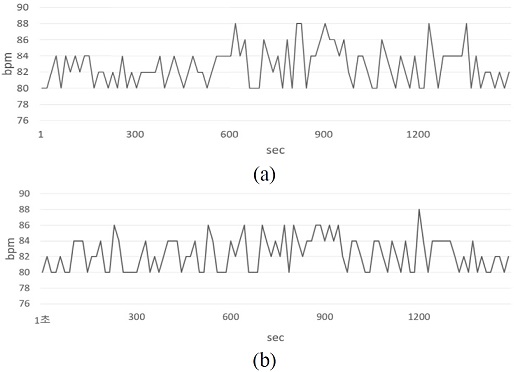
Figure 7 depicts the changes in heartbeat before and after wearing the body heat keeper. The changes before wearing it are provided in (a), whereas the changes after wearing it are provided in (b).
The average heartbeat before wearing the body heat keeper when stopped was 81.9 bpm, whereas the average heartbeat after wearing it was 81.6 bpm. The average heartbeat before wearing the body heat keeper after walking and running was 83.7 bpm, whereas the average heartbeat after wearing it was 83.4 bpm. The average heartbeat before wearing the body heat keeper after walking and stopping was 82.6 bpm, whereas the average heartbeat after wearing it was 82.2 bpm. These results demonstrated that the heartbeat was stabilized slightly more quickly after wearing the body heat keeper than before wearing it.
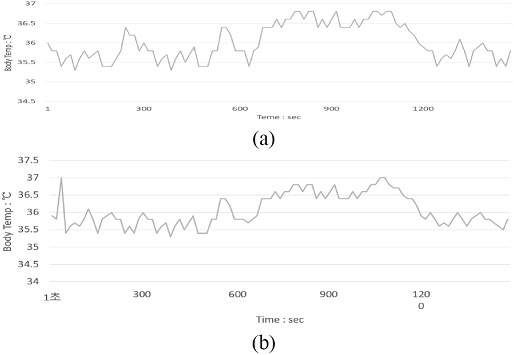
Figure 8 presents the changes in body temperature before and after wearing the body heat keeper. The changes before wearing it are provided in (a), whereas the changes after wearing it are provided in (b).
The result of comparison of the body temperature changes revealed that the average body temperature was lower by 0.1 ℃ after wearing the body heat keeper than before wearing it when the wearer ran, thereby demonstrating that, after walking and stopping, the body temperature was recovered to the normal level in a more stable manner after wearing the body heat keeper.
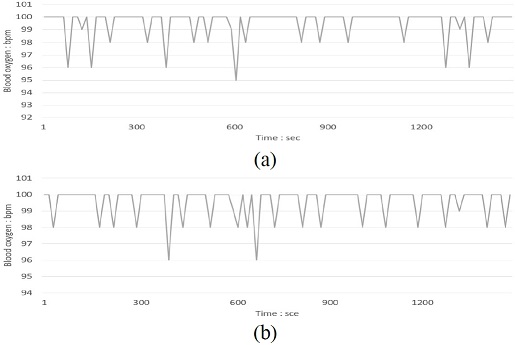
Figure 9 depicts the changes in blood oxygen before and after wearing the body heat keeper. The changes before wearing it are provided in (a), whereas the change after wearing it are provided in (b). The average blood oxygen was 99.5 bpm. Therefore, there was no significant change in blood oxygen owing to the use of the body heat keeper, similar to the heartbeat and body temperature.
Ⅴ. Conclusion
In this study, we developed a wearable device for PHR application and measured real-time changes in the device wearer’s heartbeat, blood oxygen, and body temperature. The results of the measurement of the changes in heartbeat, blood oxygen, and body temperature using the wearable device revealed that the data transfer speed appeared to be as fast as 24.0 ms. There was no significant change in heartbeat, blood oxygen, and body temperature owing to the use of the body heat keeper in the experiment wherein the measurement was performed when the wearer stopped, walked, ran, walked, and stopped, presumably because the experiment participant was a healthy normal person. It is expected that the device will produce basic data for health management of the elderly and chronic patients if it is worn by them on a daily basis. In particular, if the biometric data collected by the wearable device are linked with hospital data, it will be possible to collect and manage high-quality personal health information for improvement of the wearer’s health.
Acknowledgments
This paper is that revised and supplemented the research results supported by the Small and Medium Business Promotion Agency (S2759360) in 2019.
References
- Schimidt R F, "Heat balance and the regulation of body temperature," In Human physiology. edited et. al. New York, pp. 532-547, 1964
- Blair E, "Clinical hypothermia: physiology of hypothermia," New York McGraw-Hill Cp, pp. 13-21, 1964.
-
Erickson R A, "model of adaptation to the thermal environment," Advances in nursing science, Vol. 4(4), pp. 1~12, 1982.
[https://doi.org/10.1097/00012272-198207000-00003]

- Yi S J, "Variation of vitalsign according to timein full immersion of hot and cool bath," Journal of-eKorean Physical-erapy Science, Vol. 3(3), pp. 35-49, 1996.
- Brengleman G L, Brown A C, "Physiology and biophysics Temperature regu-lation," 19th ed. W.B. Saunders co. Philadelphia and London, pp. 1050-1064, 1965.
- Kang H S, Lim N Y, Oh S Y, Kim W O, Kim K I, Lee S H, "Fundamentals of nursing," Paju Soomoonsa, 2011.
-
Yang Y W, Chen J, Zuo S, "Thermo-element geometry optimization for high thermoelectric efficiency," Energy, Vol. 147, pp. 672-680, 2018.
[https://doi.org/10.1016/j.energy.2018.01.104]

-
Zebarjadi M, Esfarjani K, Dresselhaus S M, Ren Z F, Chen G, "Perspectives on thermoelectrics: from fundamentals to device applications," Energy Environ Sci, Vol. 5, pp. 5147-5162, 2012.
[https://doi.org/10.1039/C1EE02497C]

-
Schlitz R A, Brunetti R G, Glaudell A M, Miller P L, Brady M A, Takacs C J, Hawker C J, Chabinyc M L, "Solubility‐Limited Extrinsic n.Type Doping of a High Electron Mobility Polymer for Thermoelectric Applications," Advanced Materials, Vol. 26, pp. 2825-2830, 2014.
[https://doi.org/10.1002/adma.201304866]


1992년 : 조선대학교 유전공학과 졸업 (공학사)
2001년~2010년: 진택
2009년~현 재: ㈜프로진
2020년~현 재: 동신대학교 전기전자공학과 석사과정
※관심분야: 디지털콘텐츠 시스템, 콘텐츠 응용 및 기타 융합기술, 융합콘텐츠, 의료영상, 의공학, 3D 모델링 등

2003년 : 동신대학교 대학원 (공학석사)
2006년 : 동신대학교 대학원 (공학박사-전기전자공학)
2008년 : 조선대학교 대학원 (의학박사-외과학)
2006년~2008년: ㈜바이오아테코
2008년~2010년: ㈜에코레이
2010년~현 재: 동신대학교 보건행정학과 교수
※관심분야: 디지털콘텐츠 시스템, 콘텐츠 응용 및 기타 융합기술, 융합콘텐츠, 의료영상, 의공학, 3D 모델링 등