Optimal temperature maintenance of a transfusion cooling system using thermoelement
Copyright ⓒ 2019 The Digital Contents Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-CommercialLicense(http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.

Abstract
For bleeding or disease treatment, a blood product is often received. According to the storage regulation of a blood product using platelets, a blood product should keep its temperature at 22±2°C and stir continuously. In particular, if its temperature fails to remain, cells are so influenced that they are dead or change their properties. Therefore, this study designed and developed a transfusion cooling system using thermoelement in order to maintain a storage temperature during the transfusion of a blood product and analyzed the characteristics of temperature and voltage-current. The cooling system for a transfusion can control switching to continuously change if the voltage-current polarity of thermoelement reaches a setup temperature. As a result, the internal temperature of the transfusion cooling system and the temperature of saline solution pack were able to remain at 22±2°C constantly.
초록
출혈이나 질병의 치료를 위해 혈액제제를 수혈 받는 경우가 많이 있다. 혈소판을 이용한 혈액제제의 보관 규정을 보면 22±2°C를 유지하며 지속적인 교반이 필요하다. 특히, 온도가 유지되지 않으면 세포에 영향을 끼쳐 세포가 사멸하거나 특성이 변하게 된다. 따라서 본 연구에서는 혈액제제를 수혈하는 동안에도 보관 온도를 유지 할 수 있도록 열전소자를 사용하여 수혈용 냉각장치를 설계·개발하고 온도 및 전압-전류 특성을 분석하였다. 수혈용 냉각장치는 열전소자의 전압-전류의 극성이 설정온도에 도달하면 지속적으로 변화될 수 있도록 스위칭 제어를 하였다. 그 결과 수혈용 냉각장치의 내부 온도 및 생리식염수 팩의 온도가 22±2°C의 온도를 지속적으로 유지할 수 있었다.
Keywords:
Thermo-element, Biological safety, Blood temperature maintenance, Temperature sensing, PT 100Ω sensor, Peltier effects키워드:
열전소자, 생물학적 안전, 혈액온도유지, 온도감지, PT100Ω센서, 펠티어효과Ⅰ. Introduction
If a transfusion is needed for severe bleeding or a disease, a transfusion using homologous blood is mainly given. However, an enough amount of blood is not supplied since it is very hard to secure blood through donation and to meet storage and transfer conditions. Therefore, a diversity of research on artificial blood[1]-[3]. and artificial blood vessels[4]-[7]. have been conducted. In particular, a HBOC product that can replace red blood cells was developed and is about to be applied to the human body[8]. Blood is segmented in various forms for storage. A storage temperature can influence the functional activation of blood. A platelet product is dead at a low temperature because of its failure to keep cytoskeleton[9], and changes cytoplasm at a high temperature. For this reason, the development of a device for keeping a temperature at the time of extracting PRF from blood has been researched[10]. To transfer or use blood and a blood product, it is very important to keep a temperature. In particular, when a blood or platelet product transfusion is given in an operating room, it is hard to keep a temperature. In case of a transfusion of platelets, the transfusion should be given within 30 minutes. Although the platelet transfusion is shorter than transfusions of other blood products, it is sensitive to temperature. For this reason, it is necessary to come up with a plan for keeping a temperature. Therefore, this study developed a small temperature maintenance device which is available in an operating room and analyzed temperature characteristic. To develop the temperature maintenance device, thermoelement was utilized. Thermoelement uses the inter-conversion of heat and electricity and produces various effects[11]. The temperature maintenance device makes use of Peltier effect. In terms of Peltier effect, when a current flows in P-N thermoelement, exothermic reaction occurs in one side, and endothermic reaction occurs in the other side [12],[13]. Since thermoelement has a simple structure and high reliability, it is researched a lot and is applied to real life[14]-[17]. In particular, thermoelement is utilized to make a cooling device which is often applied to homes or industries which need temperature control [18],[19]. This study developed a temperature maintenance device to keep a temperature when a transfusion is given in an operating room and analyzed its characteristics.
Ⅱ. Materials and Methods
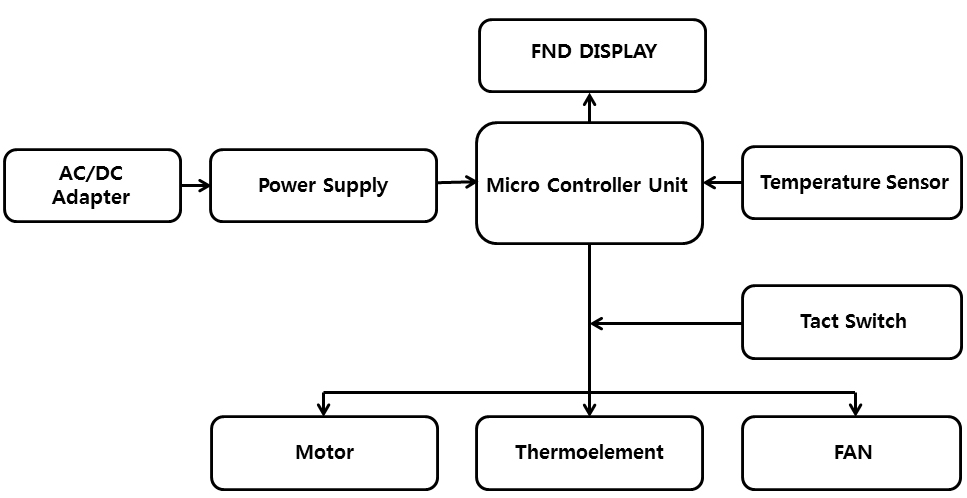
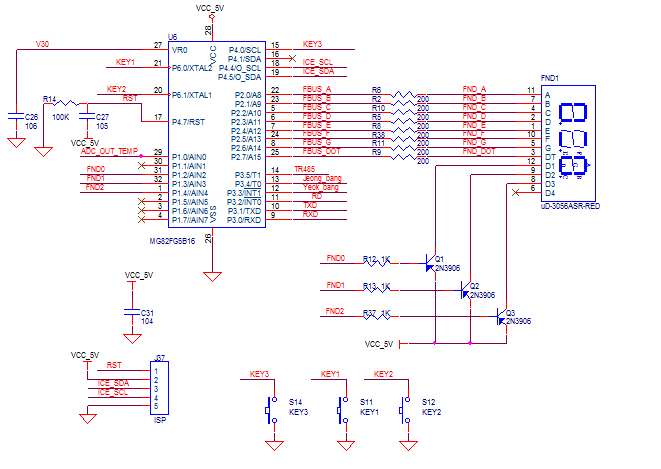
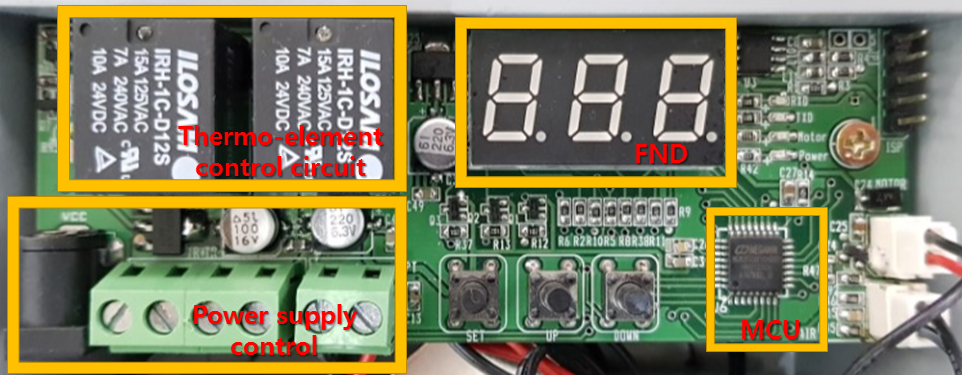
The cooling device for a transfusion is comprised of Micro Controller Unit (MCU) that controls the cooling device for a transfusion, the thermoelement part that helps to keep a temperature of a transfusion pack, and the power supply part that supplies power to the cooling device for a transfusion. Micro Controller Unit plays a role to control the whole cooling device for a transfusion. MCU sends a drive signal of thermoelement(TEC1-12706, YUXIANG electronics China) to keep a proper temperature. The MCU can also control the switch (NW3-TS-D005, NW3 corp, China) to drive the vibration motor (SZH-GNP131, SMG corp, China) and the pan (DA12025S12LA, Shenzhen huaxia hengtai electronic corp, China). The drive voltage of the MCU(MG82FG5B16, MEGAWIN corp, China) is 5V and its current is 6A. The transfusion cooling device supplies power with the use of the adaptor (SWpp-12604000-w, Hongkong power-tek international corp, China). For temperature control of the transfusion cooling device, the temperature sensor (NTC-103F397, SAMKYUNG corp, korea) was used. The detected temperature data was transmitted to the MUC with the use of ADC(Analog to Digital Converter). The screen display utilized FND(S-5363ASR1, DAKWANG corp, Chin) to display up to three digits of the current temperature.
The MCU of the transfusion cooling device has the structure of 8-bit RISC so that it has simple commands. Also, it has low power consumption, since pull-up resistance is selectable. The display of the transfusion cooling device is designed with the use of FND. In FND, the internal temperature value is presented in real time. It is possible to select thermoelement operation, vibration motor operation, and pan operation with the use of three switches. As a temperature sensor, the NTC(Negative Temperature Coefficient)-thermistor temperature sensor is used. The NTC temperature sensor utilizes its characteristic of a resistance value changing depending on a temperature. It calculates a resistance value with the use of its temperature table in the principle of voltage distribution and then finds a temperature on the basis of the resistance value.
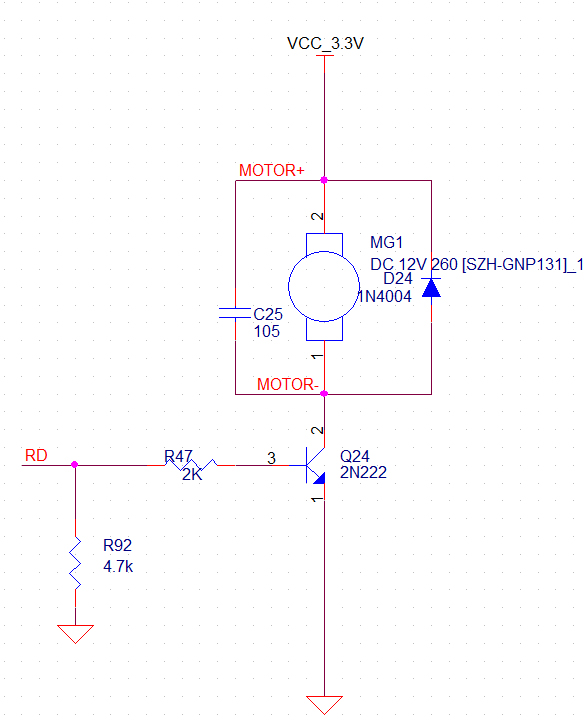
Figure 3 illustrates the circuit diagram of the vibration motor of the transfusion cooling device. A platelet product needs to stir in case of storage. In a transfusion of a platelet product, instead of stirring, the vibration motor was used to shake the platelet product. The vibration motor was turned on or off with the use of 2N2222 transistor, and its switching control was made with the MCU.
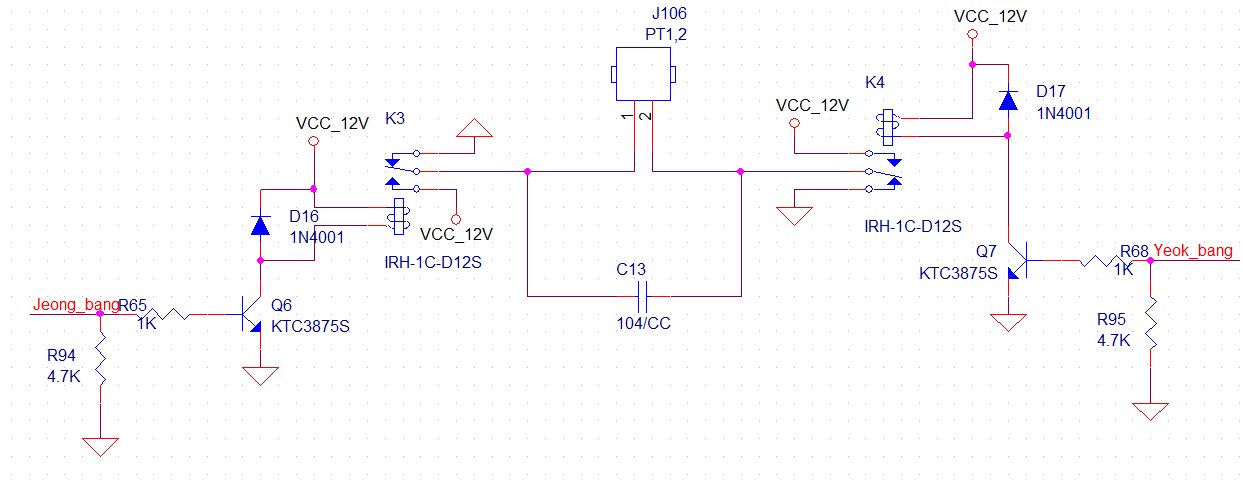
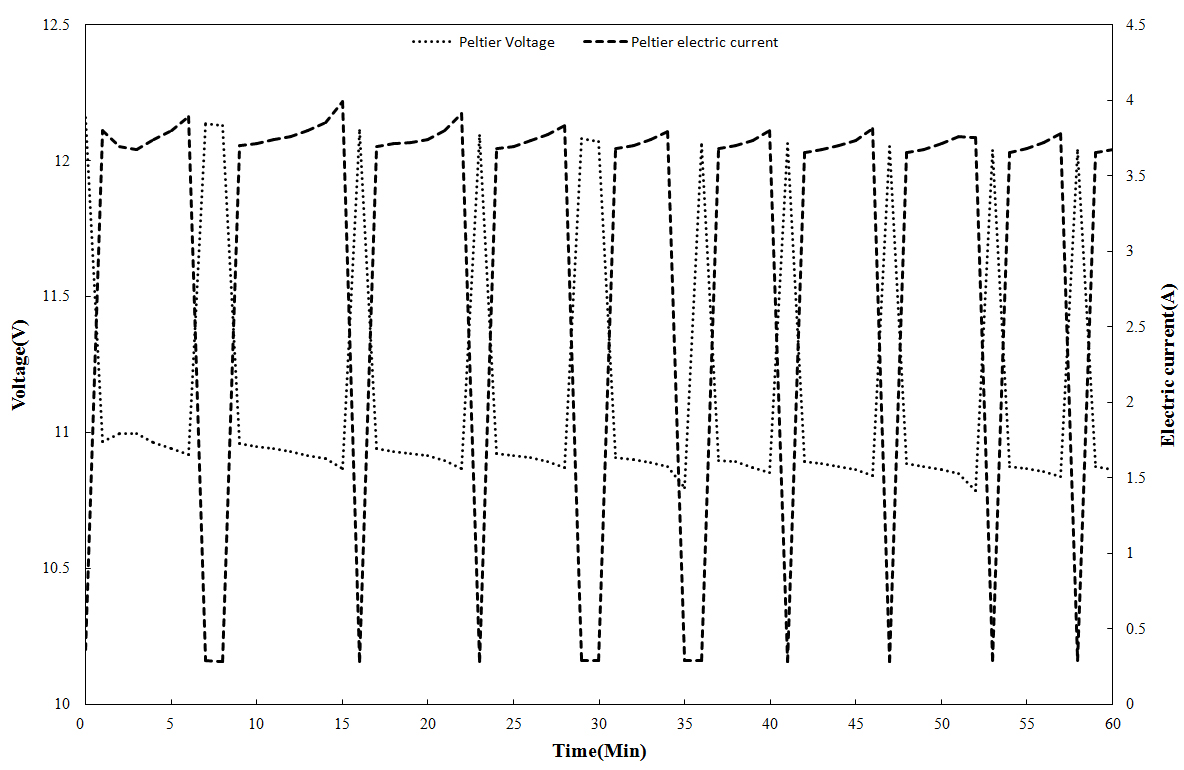
Figure 4 illustrates the circuit diagram of the thermoelement control of the transfusion cooling device. The transfusion cooling device was designed in rated control with the use of a relay, since its internal space was narrow. The drive current of one Peltier device is about 6A. For this reason, a relay with 10A of the maximum allowable current was utilized to drive the thermoelement in a stable way. Q6 transistor was turned on and Q7 transistor was turned off so as to supply +12V and give cooling control to the thermoelement. On contrary, it was possible to supply –12V and give heat control to the thermoelement by turning of Q6 transistor and turning on Q7 transistor. In order to emit the internal air of the transfusion cooling device quickly and cool the thermoelement, a heatsink and a pan were attached. With respect to the blood product transfer system, thermo-elements that could provide cooling and heating control according to the variation of the polarity of the current were used to maintain a specific temperature in a variable external temperature environment.
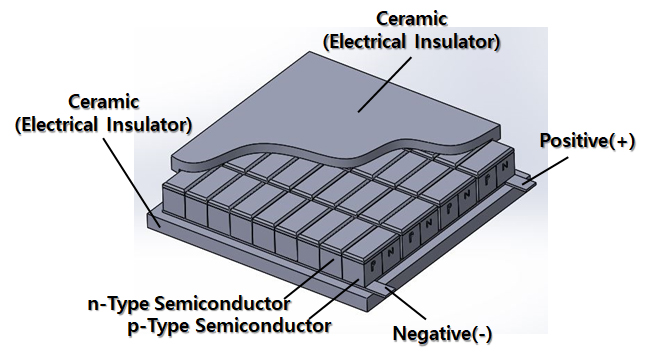
Figure 5 illustrates the structure of a thermo-element. This is comprised of thermo-element semiconductors with p-type and n-type, a ceramic plate for electric insulators, and a two-way connector. The thermo-element has a type of pn joining. Therefore, by connecting multiple p-type and n-type semiconductors, it is possible to make a variety of devices with a different size depending on use purposes[14],[15],[19]. The thermo-element has Seebeck effect, Peltier effect, and Thomson effect[20]. This study made use of the Peltier effect in which one side of a thermo-element absorbs heat and the other side emits heat in order to control the temperature of the blood product transfer system. Table 1 presents the specification of the thermo-element (TEC1-12706, Hebei IT corp., China) used in this study.
Ⅲ. Results
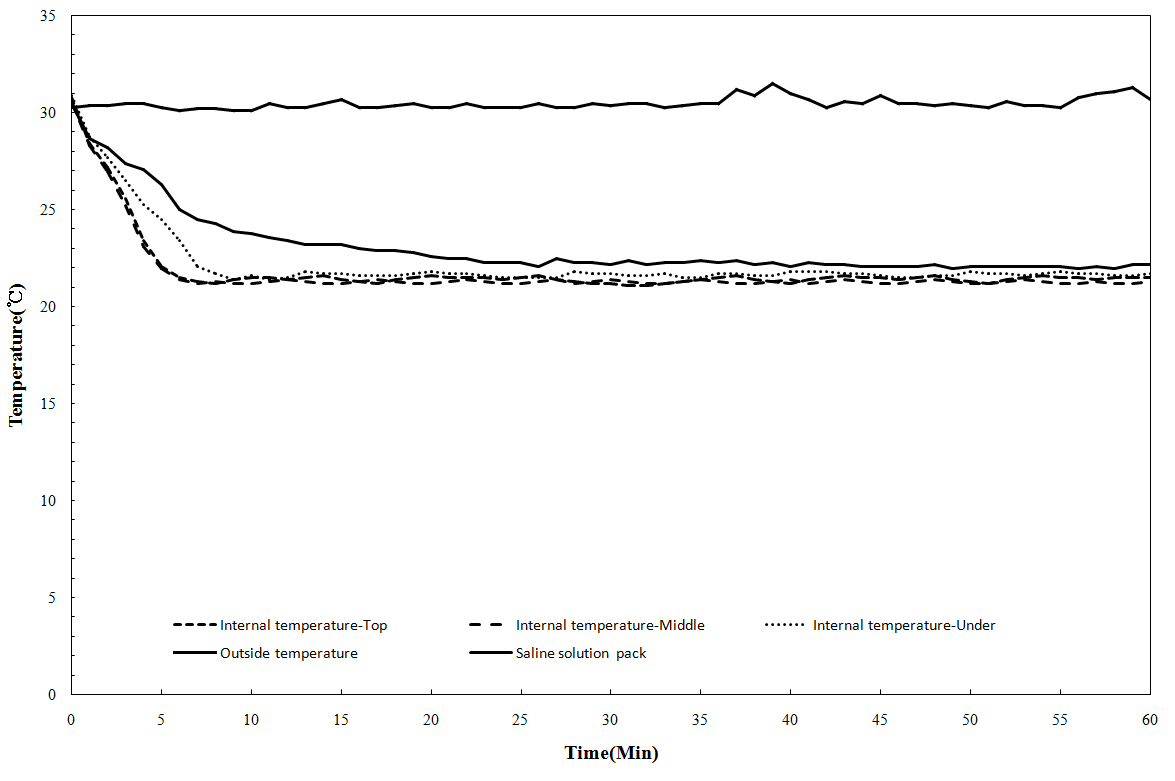
Figure 6 was the Printed circuit board (PCB) designed to control temperature change of the transfusion cooling device. Figure 7 presents the temperature change of the transfusion cooling device. A temperature sensor was attached to the top and bottom in the transfusion cooling device, its vibration motor, and its saline solution pack in order to analyze a change in the internal temperature of the transfusion cooling device. An outside temperature was set to more than 30℃. To check that the internal temperature of the transfusion cooling device was uniform, the temperature sensors were attached to the top and bottom of the device sion, and a temperature was measured. For temperature measurement, the data logger (GL240, Graphtec corp, Japan) and the K-type temperature sensor (TP-K01, Lab&Tools corp, Korea) were used for one hour after transfusion cooling device was operated. The temperature of transfusion cooling device should remain at 22±2°C, the storage reference of a platelet product. Since the outside temperature was very high, or more than 30°C, its internal temperature was more than 30°C even if the transfusion cooling device was initial operation. However, the temperature remained at 22±2°C. It was found that the transfusion cooling device was smoothly operated in a space with a high outside temperature. If the temperature of a platelet product fails to remain in a certain level, cytoplasm changes and it is impossible to keep the properties of the product. Therefore, it is required to keep a uniform temperature.
Figure 8 presents the voltage-current change of the transfusion cooling device when a thermoelement runs for temperature maintenance. For voltage-current measurement, the data logger was used through the power unit connected to thermoelement. If the transfusion cooling device starts to run, a thermoelement also begins to run to keep a temperature at 22±2°C. If an outside temperature is high, cooling starts; if lower than a setup temperature, cooling stops. After cooling stops, the thermoelement changes the polarity of a current and starts to heat in order to maintain a temperature. The device was designed to keep a temperature at 22±2°C as a setup temperature through repeated process. In other words, depending on a setup temperature of the transfusion cooling device, thermoelement repeatedly makes switching control to keep an internal temperature stable. As the thermoelement starts to run, voltage-current changes in a certain pattern due to the switching control of thermoelement. It means that the polarity of voltage-current changes continuously to find a setup temperature. The thermoelement had heating-cooling operation continuously and was able to keep a temperature at its target internal temperature ‘22±2°C’ about six minutes after the transfusion cooling device was operated. After about 10 minutes, the saline solution pack also kept a temperature at 22±2°C. A platelet product needed about 30 minutes of transfusion. Therefore, if a transfusion starts 10 minutes after the operation of the transfusion cooling device, it is judged that the transfusion is able to be given at a stable temperature.
Ⅳ. Conclusion
A blood product is sensitive to a temperature change. Therefore, if such a product is not influenced by an outside temperature change and keeps a constant temperature, it is possible to give a blood product transfusion to a patient safely. This study designed and developed the cooling device for a transfusion with the use of thermoelement, and analyzed changes in internal temperature and voltage-current. The thermoelement was installed in the inside of the case of the transfusion cooling device, and a pan was installed in the outside of the case in order to cool and heat an internal temperature quickly. In order to keep a temperature at 22±2°C no matter how high an outside temperature was, the transfusion cooling device was designed for cooling and heating with the use of thermoelement. When an outside temperature was more than 30°C, an initial internal temperature was high. With the cooling operation of thermoelement, the internal temperature went down to the target temperature or 22±2°C and remained. To do that, the thermoelement had cooling and heating operation continuously, and the switching operation of the thermoelement continuously changed the polarity of voltage and current. It is expected that the thermoelement based cooling device for a transfusion is not influenced by an outside temperature change, keeps an internal temperature in a certain level, and helps to give a blood product transfusion to a patient safely.
Acknowledgments
This work (Grants No.C0443154) was supported by project for Cooperative R&D between Industry, Academy, and Research Institute funded Korea Ministry of SMEs and Startups in 2017.
References
-
A. I. Alayash, 'Hemoglobin-Based Blood Substitutes and the Treatment of Sickle Cell Disease: More Harm than Help?', Biomolecules, 7(1), p2-14, (2017).
[https://doi.org/10.3390/biom7010002]

-
M. Arkosi, F. Scurtu, A. Vulpol, and R. S. Dumitrescu, 'Copolymerization of recombinant Phascolopsis gouldii hemerythrin with human serum albumin for use in blood substitutes', Artificial Cells Nanomedicine and Biotechnology, 45(2), p218-223, (2017).
[https://doi.org/10.1080/21691401.2016.1269118]

-
Z. Tao, P. P. Ghoroghchian, 'Microparticle, nanoparticle, and stem cell-based oxygen carriers as advanced blood substitutes', Trends in Biotechnology, 32(9), p466-473, (2014).
[https://doi.org/10.1016/j.tibtech.2014.05.001]

-
H. Y. Ng, K. A. Lee, C. N. Kuo, and Y. F. Shen, 'Bioprinting of artificial blood vessels', Inter. J of Bioprinting, 4(2), 1134, (2018).
[https://doi.org/10.18063/ijb.v4i2.140]

-
H. Y. Deng, C. L. Qin, X. M. Qiu, and Q. H. Zhou, 'Successful removal of giant primary osteosarcoma in the anterior mediastinum invading the superior vena cava and right lung with artificial blood vessel reconstruction', Europ. J Cardio-Thoracic Surgery, 52(4), 828, (2017).
[https://doi.org/10.1093/ejcts/ezx168]

-
J. D. Kakisis, C. D. Liapls, C. Breuer, and B. E. Sumpio, 'Artificial blood vessel: The Holy Grail of peripheral vascular surgery', J Vascular Srrgery, 41(2), p349-354, (2005).
[https://doi.org/10.1016/j.jvs.2004.12.026]

-
D. Klemm, D. Schumann, U. Udhardt, and S. Marsch, 'Bacterial synthesized cellulose-artificial blood vessels for microsurgery', Progress in Polymer Science, 26(9), p1571-1603, (2001).
[https://doi.org/10.1016/s0079-6700(01)00021-1]

- J. H. Kim, and K. Y. Lee, 'Current Status and Future of Artificial Blood-Focusing on Red Blood Cell Substitues', J Korean Med Assoc, 52(2), p168-181, (2009).
-
J. H. Lee, J. T. Kim, and Y. G. Cho, 'Effect of Netric Oxide on the Cryopreservation of Platelets', Korean J Lab Med, 28(2), p136-43, (2008).
[https://doi.org/10.3343/kjlm.2008.28.2.136]

-
K. J. Sun, Y. T. Cho, and M. W. Cheon, 'Development of PRF extractor using thermoelectric element and temperature sensor', Sensors and Actuators A; Physical, 263, p778-782, (2017).
[https://doi.org/10.1016/j.sna.2017.05.017]

- S. H. Han, Y. J. Kim, J. H. Kim, D. J. Kim, J. Y. Jung, S. Kim, and G. S. Cho, 'Control of Heat Temperature in Light Emitting Diodes with Thermoelectric Device', Journal of the Korean Vacuum Society, 20, p280-287, (2011).
-
N. Ari, and A. Kribus, 'Impact of the Peltier effect on concentrating photovoltaic cells', Solar Energy Materials and Solar Cells, 94, p2446-2450, (2010).
[https://doi.org/10.1016/j.solmat.2010.08.015]

- C. H. Wang, and C. Y. Kuo, 'Peltier effect on CoSn3 growth in Sn/Co/Sn couples with different substrate lengths', Materials Chemistry and Physics, 153, p72-77, (2017).
- Y. G. Seo, J. S. Ko, and D. H. Chung, 'The temperature contrl of dehumiditier by thermoelectirc device using SPI controller', J KIIEIE, 32(4), p87-94, (2018).
-
Y. Wu, J. Yang, S. Cheon, and L. Zuo, 'Thermo-element geometry optimization for high thermoelectric efficiency', Energy, 147, p672-680, (2018).
[https://doi.org/10.1016/j.energy.2018.01.104]

- M. Zebarjad, K. Esfarjani, M. S. Dresselhaus, Z. F. Ren, and G. Chen, 'Perspectives on thermoelectrics: from fundamentals to device applications', Energy & Environmental Sci, 5, p5147-5162, (2012).
- R. A. Schlitz, F. G. Brunetti, A. M. Glaudell, P. L. Miller, M. A. Brady, C. J. Takacs, C. J. Hawker, and M. L. Chabinyc, 'Solubility‐Limited Extrinsic n‐Type Doping of a High Electron Mobility Polymer for Thermoelectric Applications', Advanced Materials, 26, p2825-2830, (2014).
-
A. Martinez, D. Astrain, A. Rodriguez, and P. Aranguren, 'Advanced computational model for Peltier effect based refrigerators', Applied Thermal Engineering, 95, p339-347, (2016).
[https://doi.org/10.1016/j.applthermaleng.2015.11.021]

-
M. Liao, X. He, C. Jiang, X. Fan, Y. Li, and F. Qi, 'A three-dimensional model for thermoelectric generator and the influence of Peltier effect on the performance and heat transfer', Applied Thermal Engineering, 133, p493-500, (2018).
[https://doi.org/10.1016/j.applthermaleng.2018.01.080]

- Yu, S. Y., Hong, J. P., Sim, W. S., A study on the performance of thermoelectric module and thermoelectric cooling system, Int. J. Air Conditioning and Refrigeration, 16, p62-69, (2004).

1989년 : 경상대학교 간호학사
1998년 : 경상대학교 간호학석사
2005년 : 부산대학교 간호학박사
1989년~2006년: 인제대학교 부산백병원
2007년~현재: 광주보건대학교 간호학과 교수
※관심분야: 의료정보, 감염관리, 병원경영 등

2008년 : 조선대학교 대학원 (의학박사)
2006년 : 동신대학교 대학원 (공학박사)
2006년~2008년: (주)바이오아테코
2008년~2010년: (주)에코레이
2010년~현 재: 동신대학교 보건행정학과 교수
※관심분야: 의료영상, 의공학, 3D 모델링 등